What is Chronic Fatigue Syndrome?
Chronic Fatigue Syndrome (CFS), also known as Myalgic Encephalomyelitis (ME), is a complex and debilitating medical condition characterized by persistent and unexplained fatigue that is not improved by rest. The fatigue is often severe and can be accompanied by a range of other symptoms, which may vary from person to person.
The exact cause of chronic fatigue syndrome is not fully understood, and it is likely that multiple factors contribute to its development. Possible triggers include viral infections, immune system dysfunction, hormonal imbalances, and psychological stress.
Diagnosis can be challenging, as there are no specific laboratory tests or imaging studies that definitively identify CFS. Instead, healthcare providers typically rely on a thorough medical history, physical examination, and exclusion of other possible medical and psychological conditions.
Management of chronic fatigue syndrome often involves a multidisciplinary approach, including rest, lifestyle adjustments, cognitive-behavioral therapy, and, in some cases, medication to address specific symptoms. It’s important for individuals with CFS to work closely with healthcare providers to develop a personalized treatment plan.
What causes Chronic Fatigue Syndrome?
The exact cause of CFS is not well understood, and it is likely that a combination of factors contributes to its development. Some of the proposed factors include:
- Viral or Infectious Agents: Some researchers have explored the possibility that viral or other infectious agents could trigger or contribute to CFS. However, no specific pathogen has been consistently identified.
- Immune System Dysfunction: There is evidence suggesting that the immune system may play a role in CFS. Abnormalities in immune system function have been observed, but it’s unclear whether these are a cause or a consequence of the syndrome.
- Neurological Factors: Dysfunction in the central nervous system has been proposed as a possible cause. Changes in certain neurotransmitters and abnormalities in brain structure and function have been observed in some individuals with CFS.
- Hormonal Imbalances: Some studies have suggested that abnormalities in hormonal levels, particularly related to the hypothalamic-pituitary-adrenal (HPA) axis, may contribute to the development of CFS.
- Genetic Predisposition: There is some evidence that genetic factors may contribute to an increased susceptibility to CFS. However, no specific genetic markers have been consistently identified.
- Psychological Factors: While psychological stress and mental health conditions can contribute to fatigue, it’s essential to note that CFS is not a purely psychological disorder. However, stress and other psychological factors may play a role in exacerbating symptoms in some individuals.
- Mitochondrial Dysfunction: Some researchers have proposed that dysfunction in cellular energy production, particularly in the mitochondria, may contribute to the fatigue experienced by individuals with CFS.
Management of CFS involves a personalized and multidisciplinary approach that addresses the specific symptoms and challenges faced by each individual. This may include lifestyle adjustments, cognitive-behavioral therapy, graded exercise therapy, and medications to manage symptoms such as pain or sleep disturbances.
What are the symptoms of Chronic Fatigue Syndrome?
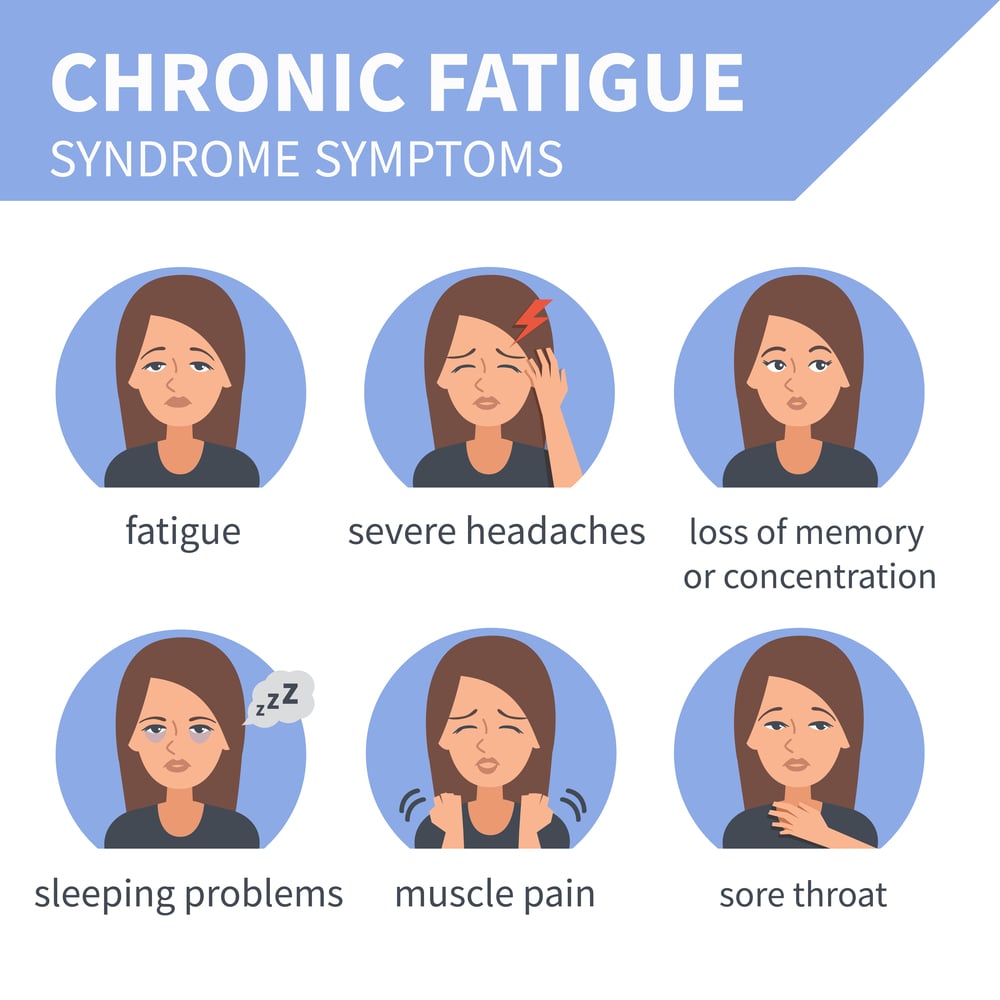
CFS is characterized by a range of symptoms that can vary in severity and may fluctuate over time. Individuals with CFS may experience a combination of the following symptoms:
- Post-Exertional Malaise (PEM): Symptoms can worsen after physical or mental exertion, often with a delay. This exacerbation of symptoms can last for days or even weeks.
- Sleep Disturbances: Despite the profound fatigue, many individuals with CFS experience sleep disturbances, such as insomnia, unrefreshing sleep, or changes in sleep patterns.
- Cognitive Dysfunction (Brain Fog): Difficulty with concentration, memory, and cognitive processing is common. This is often referred to as “brain fog.”
- Muscle and Joint Pain: Widespread pain, including muscle pain and joint pain, is a frequent symptom.
- Headaches: Persistent or recurrent headaches, including migraines, may occur.
- Sore Throat: Some individuals with CFS report a persistent or recurrent sore throat.
- Tender Lymph Nodes: Swollen or tender lymph nodes, especially in the neck and armpits, may be present.
- Sensitivity to Light and Noise: Individuals with CFS may be more sensitive to light and noise.
- Digestive Issues: Some people with CFS may experience gastrointestinal symptoms, such as nausea or irritable bowel syndrome.
- Orthostatic Intolerance: Symptoms may worsen when standing or sitting upright, leading to dizziness or light-headedness.
It’s important to note that the severity and combination of symptoms can vary widely among individuals with CFS. Additionally, the symptoms of CFS can overlap with those of other medical conditions, making diagnosis challenging. A diagnosis is typically made after excluding other potential causes of the symptoms.
The symptoms of CFS can significantly impact daily functioning and quality of life. Management strategies often involve a multidisciplinary approach that addresses the condition’s physical and psychological aspects. It’s important for individuals experiencing these symptoms to seek medical evaluation and work with healthcare providers to develop a personalized treatment plan.
How is Chronic Fatigue Syndrome diagnosed?
Diagnosing CFS can be challenging because there are no specific laboratory tests or imaging studies that definitively identify the condition. Instead, healthcare providers rely on a combination of clinical criteria, medical history, physical examination, and the exclusion of other possible causes for the symptoms.
The process typically involves the following steps:
- Medical History and Symptom Assessment: Healthcare providers will conduct a thorough medical history to understand the onset, duration, and nature of the symptoms. They will ask about fatigue, post-exertional malaise, sleep disturbances, cognitive difficulties, and other symptoms associated with CFS.
- Physical Examination: A physical examination is performed to rule out other medical conditions and assess the overall health of the individual.
- Laboratory Tests: Blood tests may be conducted to rule out other medical conditions that can cause similar symptoms, such as anemia, thyroid disorders, autoimmune diseases, and infections. The absence of specific abnormal laboratory findings is a characteristic feature of CFS, but these tests are important for excluding other potential causes.
- Diagnostic Criteria: Healthcare providers often refer to specific diagnostic criteria to help establish a diagnosis. The Fukuda criteria, established by the Centers for Disease Control and Prevention (CDC), and the International Consensus Criteria for ME/CFS are commonly used.
- Exclusion of Other Conditions: CFS is a diagnosis of exclusion, meaning that other medical and psychological conditions with similar symptoms must be ruled out. This may involve additional testing or consultations with specialists.
- Consultation with Specialists: Depending on the symptoms and findings, individuals may be referred to specialists such as rheumatologists, infectious disease specialists, or neurologists for further evaluation.
Is Chronic Fatigue Syndrome A Disability?

Yes, chronic fatigue syndrome (CFS) can be considered a disability, and individuals with severe cases of CFS may experience significant limitations in their daily functioning. In many countries, including the United States, the United Kingdom, and others, CFS is recognized as a medical condition that can lead to disability.
The severity of CFS can vary widely among individuals, and some people with CFS may be able to manage their symptoms and continue with their regular activities to some extent, while others may find it extremely challenging to carry out basic tasks. Individuals with CFS often experience persistent and unexplained fatigue, along with other symptoms such as pain, cognitive difficulties, and sleep disturbances.
The impact of CFS on a person’s ability to work and engage in other daily activities can be substantial. In some cases, individuals with CFS may qualify for disability benefits or accommodations at work, depending on the severity of their symptoms and the specific regulations in their country.
It’s important for individuals with CFS who are experiencing significant limitations to consult with healthcare professionals and, if necessary, with legal and employment experts who can provide guidance on disability-related matters. In some cases, individuals may need to work with healthcare providers to document the severity and impact of their condition for disability benefit applications or workplace accommodations.
The specific criteria for disability benefits and accommodations can vary by country and region, so individuals should be familiar with the relevant laws and regulations in their location. Additionally, working with healthcare professionals and legal experts can help individuals navigate the process of seeking disability accommodations or benefits.
Chronic Fatigue Syndrome Treatment:
The treatment of CFS typically involves a multidisciplinary and individualized approach, as symptoms can vary widely among individuals. There is no cure for CFS, so the focus is often on managing symptoms and improving quality of life.
Here are some common components of CFS treatment:
- Symptom Management: Individuals with CFS often find it helpful to pace themselves, balance activities, and rest to avoid overexertion. This can help prevent post-exertional malaise, a worsening of symptoms after physical or mental exertion. Establishing good sleep habits and addressing sleep disturbances is an important aspect of managing CFS. This may involve creating a consistent sleep schedule, creating a restful sleep environment, and avoiding stimulants close to bedtime.
- Cognitive-Behavioural Therapy (CBT): CBT is a type of psychotherapy that can be beneficial for individuals with CFS. It focuses on changing negative thought patterns and behaviors that may contribute to symptom exacerbation. CBT can help individuals cope with the challenges of living with a chronic illness.
- Graded Exercise Therapy (GET): Under the guidance of a healthcare professional, individuals may gradually increase their physical activity level. This is done in a systematic and individualized manner to avoid triggering post-exertional malaise.
- Medication: Medications may be prescribed to manage specific symptoms, such as pain, sleep disturbances, or other associated conditions. The choice of medication depends on the individual’s symptoms and needs.
- Diet and Nutrition: Maintaining a balanced and nutritious diet can support overall health. Some individuals with CFS may find that dietary modifications, such as avoiding certain foods or additives, can help alleviate symptoms.
- Stress Management: Managing stress is important for individuals with CFS. Techniques such as mindfulness, relaxation exercises, and stress-reduction strategies can be beneficial.
- Supportive Therapies: Physical therapy, occupational therapy, and other supportive therapies may be recommended to address specific symptoms and improve overall functioning.
Chronic Fatigue Syndrome Medication:
There is no specific medication that universally cures CFS, but medications may be prescribed to manage specific symptoms associated with the condition. It’s important to note that the choice of medication is based on individual symptoms and needs, and treatment plans are often tailored to each person’s situation.
Here are some medications that may be considered in the management of CFS:
- Pain Medications: Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) can help reduce pain and inflammation associated with CFS. Acetaminophen may be used for pain relief, but it doesn’t have anti-inflammatory properties.
- Sleep Medications: Sedative-Hypnotics medications such as Zolpidem (Ambien) or Trazodone may be prescribed to improve sleep in individuals with CFS who are experiencing sleep disturbances.
- Antidepressants: Selective Serotonin Reuptake Inhibitors (SSRIs) or Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) such as Fluoxetine or Venlafaxine (Effexor), may be prescribed to manage symptoms of depression and anxiety, which can often coexist with CFS. Tricyclic Antidepressants (TCAs) such as Amitriptyline, may be used to manage pain and improve sleep.
- Antiviral Medications: In some cases, antiviral medications may be considered if there is evidence of a recent viral infection triggering CFS. However, using antivirals in CFS is controversial, and more research is needed to establish their effectiveness.
- Symptom-Specific Medications: Medications may be prescribed to address specific symptoms, such as headaches, migraines, or orthostatic intolerance (difficulties standing upright).
Endnote:
In conclusion, we recognize the challenges posed by CFS and the need for a compassionate and comprehensive approach to its management.
By fostering understanding, advocating for research, and supporting individuals with CFS, we can collectively contribute to improving the quality of life for those affected by this complex condition.
FAQs:
Is chronic fatigue syndrome real?
Yes CFS is a real and well-recognised syndrome.
How long does chronic fatigue syndrome last?
CFS can last from 2 weeks to 6 months.
Can herpes cause chronic fatigue syndrome?
Yes, herpes can cause CFS.
Is chronic fatigue syndrome an autoimmune disorder?
Yes, there is some evidence of chronic fatigue relating to autoimmune disorders.
Can COVID cause chronic fatigue syndrome?
Studies have suggested that COVID can cause this chronic fatigue syndrome to develop in humans.